WCC Nursing Mission Statement
The mission of the nursing programs of the Alabama Community College System is to prepare graduates to practice safe, competent, patient-centered care in an increasingly complex and rapidly changing health care system. We seek to provide full and equal access to opportunities for education success to meet the community needs.
Nursing Philosophy
We believe that nursing is a dynamic profession, blending science with the use of evidence based practice and clinical reasoning and the art of caring and compassion to provide quality, patient-centered care.
We believe learning is an interactive process in which faculty and students share responsibility to meet program outcomes. We believe in using educational methods that are current and supportive of students in the teaching and learning environment, with the presentation of information from simple to complex.
Nursing is guided by standards of practice and standards of professional performance. Standards reflect the values and priorities of the nursing profession. Therefore, we have integrated competencies from the Quality and Safety Education for Nurses (QSEN) and National League of Nursing (NLN) into our philosophy as part of our core values.
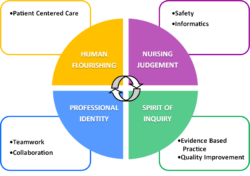
Conceptual Framework
The conceptual framework derived, from the philosophy, forms a basis for the organization and structure of the nursing curriculum. This framework serves as a guide for nursing instruction in the attainment of student learning outcomes.
The framework consists of concepts that encompass the qualities of a successful graduate nurse. NLN competencies were chosen because they specifically define the competencies of the graduate Associate Degree Nurse. QSEN competencies reflect current contemporary practice. Concepts interlace NLN and QSEN competencies to achieve the goal of providing graduate nurses with the tools needed to provide holistic care in an ever-changing health care delivery system. Each competency includes knowledge, skills, and attitudes to serve as a basis for consistent performance expectations across academic.
Competencies
NLN competencies for nursing are central to the conceptual framework. The related QSEN competencies for graduate nurses define the knowledge, skills, and attitudes that the graduate nurse should possess to continuously improve the quality and safety of the healthcare systems within which they work. (QSEN)
- Human Flourishing – Advocate for patients and families in ways that promote their self-determination, integrity, and ongoing growth as human beings. (NLN, 2022)
- Patient-Centered Care – Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values and needs. (QSEN, 2020)
- Nursing Judgement – Make judgements in practice, substantiated with evidence, that integrate nursing science in the provision of safe, quality care and that promote the health of patient within the family and community context. (NLN, 2022)
- Safety – Minimizes risk of harm to patients and providers through both system effectiveness and individual performance. (QSEN, 2020
- Informatics – Use of information and technology to communicate, manage knowledge, mitigate error, and support decision making. (QSEN, 2020)
- Professional Identity – Implement one’s role as a nurse in ways that reflect integrity, responsibility, ethical practices, and an evolving identity as a nurse committed to evidence-based practice, caring, advocacy, and safe, quality care for diverse patients within a family and community context. (NLN, 2022)
- Teamwork and Collaboration – Function effectively within nursing and inter-professional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. (QSEN, 2020)
- Spirit of Inquiry – Examine the evidence that underlies clinical nursing practice to challenge the status quo, questions underlying assumptions, and offer new insights to improve the quality of care for patients, families, and communities. (NLN, 2022)
- Evidence-based Practice – Integrate best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care (QSEN, 2020)
- Quality Improvement – Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems. (QSEN, 2020)